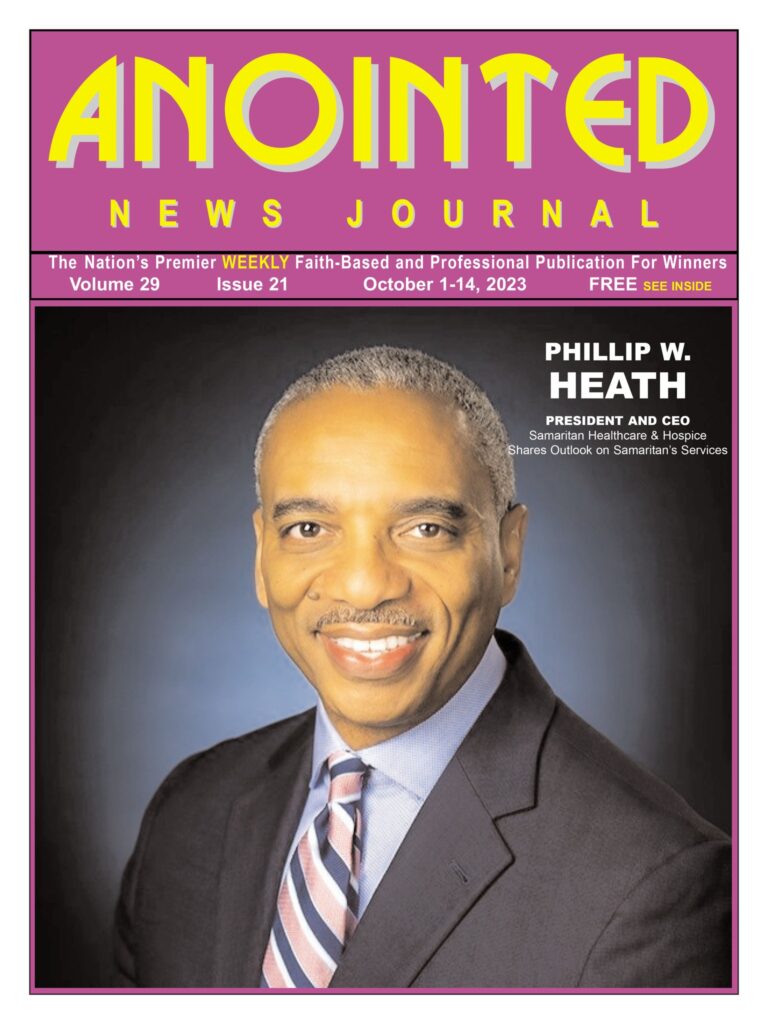
Phillip W. Heath, President and CEO of Samaritan Healthcare & Hospice, is a compassionate and dedicated figure in the field of healthcare, particularly in the realm of hospice care. This deep-seated affinity for helping the elderly has been the cornerstone of his remarkable 32-year career.
In an exclusive interview with the nation’s faith-based and professional newspaper for winners, Anointed News Journal, Phillip W. Health shares his outlook on end of life care, and how his organization is helping families.
Collins:
Share with us who is Philip W Heath. Okay.
Heath:
Well, thank you very much, Chris. I appreciate this time. So it’s interesting. I’m actually not a native of New Jersey. I’m actually a native of Michigan. I grew up in the Detroit area and spent most of my growing up years in a very large family. Seventh of eight, finished my primary and high school years in Michigan, and then I moved to Georgia, where I attended Morehouse College in Atlanta, Georgia. And then from there I went back to Michigan and pursued my graduate work at the University of Detroit, Mercy. All of my life I have had an interest in helping people, particularly older people. I guess, fortunately and unfortunately, I never really knew my grandparents. They had passed away before I was born, with the exception of my mother’s parents, but passed shortly after I was born. And so I just have always had this affection for older people and my life work has always been somewhere in and around older people.
Collins:
And you’re also a family man?
Heath:
I am, yes. My wife of almost 30 years and I met in college. She’s a Spelman College graduate. And so we met while we were in college. I have one son, and he and his wife are expecting their first child.
Collins:
Congratulations. You are also the president, CEO of Samaritan Healthcare & Hospice. What motivated you to pursue a career such as where you are today?
Heath:
Very interesting motivations. As I indicated, I’ve always loved working with elderly, supporting elderly population most of my health care career. My first job was in a hospital in Michigan, and I was working in a pharmacy and then eventually started working in their senior wellness program and started working with senior citizens in our community. When I was in graduate school, my graduate advisor knew of my interest in working with elderly and told me about an opportunity to start working with a hospice organization. And I was excited until they told me that it was not in Michigan. I thought I was going to be in Michigan all of my life, but when they told me that it was in Florida, I got really excited because I thought I’d never shovel snow again. And so I took a job working for a hospice company in Miami, Florida, in 1991. And that was really the beginning of my entrance into hospice in particular, and then spent the last 32 years working with either hospice or elderly people who need it.

End of life type services such as individuals who lived in assisted living, individuals who worked in programs of all inclusive care for the elderly, sometimes referred to as a “life programs”, living independently for elders. So my career in hospice really spans about 32 years and sort of right out of graduate school. But prior to that, I had always worked in and around people in health care or older people.
Collins:
Hospice is something that’s often misunderstood in the urban communities. What exactly is hospice and is there or what is the difference between hospice and end of life care, which you mentioned?
Heath:
So I think that so I’ll respond to a couple of things. So one is, yes, particularly in urban communities and communities of color, there’s always been this misunderstanding around hospice, but I don’t think it’s just hospice by itself. I think it’s health care in general. And for those of us who know a little bit of history, we have seen a lot of communities of color disenfranchised or abused in response to health care. We’ve seen the issues with Henrietta Lacks. We’ve seen the issues with the syphilis project and so individuals can look those up. But those were issues that were pivotal in our care over the years. And it really goes even back further than that. So I think that there’s just a trust factor associated with that. But beyond that, one of the things that also challenges urban communities in particular and communities of color in general, when you think of race and ethnicity and the roots of our community, we take care of our families. We don’t really send our family members to an institution someplace. We keep them in our home and we care for them.
And so that is actually the beauty of hospice in that you are in your home and individuals do not leave their home for hospice care. A hospice is provided primarily in an in-home setting, and then if the in-home setting gets complicated, we do have inpatient settings where people may go to a care center like the one Samaritan has in Voorhees and in Mount Holly, New Jersey. But hospice is really designed for people who are struggling with serious illness, people who need support, whether it’s with cancer or another life limiting illness or even the dementia type or Alzheimer’s type, those things are very important to receive additional support and care.
What I always tell people is palliative care is not hospice care. It’s really pain management and support of symptoms related to pain management. Not all palliative care is hospice, but all hospice is palliative care. And so hospice is there for those additional support services. Those additional support services are provided through an interdisciplinary team. And for individuals who don’t understand what that means, it really means you have a doctor, you have a nurse, you have a social worker, volunteers, spiritual care chaplains support to help you with your end of life crisis. And we say end of life a lot of times; end of life support because at some point everyone meets that date in their life at the end and it could be early or late. But we’re here to support individuals at any time to be able to support them. And then Samaritan has actually grown actually beyond just hospice services in particular.
Collins:
I want to ask you about that. I’m glad that you mentioned some of the alternatives. Because my father suffered with Alzheimer’s for like seven years. And as a family of six of us, we could not afford adult day care at that time if it even existed. So we did not know that he would have qualified for hospice. Oftentimes in communities of color, we think hospice is the very end. So what do you say to people and people of color when it comes to hospice? At what point should they try to acquire care for their loved ones?
Heath:
You know, my recommendation is the earlier you call, the more we can help. And what I mean by that is sometimes, especially if you’re not a medical professional, you just need someone to at least assess the situation, to identify what are the needs. And sometimes it may be just palliative support, it may be home and community based support, or it may be full-on hospice support. And I think that by allowing their health professionals as well as themselves to be involved in that dialogue, I think that it helps the families. It takes the burden off the family where the family can really be just the daughter, the son, the wife or the husband that they need to be, and allow the health care professionals to help you navigate that. Because we all know health care, whether you’re a person of color or not, it’s a complicated industry. It’s a complicated service for many people. And just trying to understand it. The beauty is that if someone is receiving hospice care and they’re Medicare age and even Medicaid Eligible is covered 100%. And so that is something that’s important. And then as I shared as part of Samaritan, there are some above and beyond services that we provide that aren’t necessarily in the traditional Medicare Medicaid reimbursement, but those are services that are important that we provide our community.
Collins:
And Samaritan certainly is one of the more familiar agencies when it comes to hospice care. But let’s talk about your expansion into other areas of service.
Heath:
Well, thank you for that question. So the expansion in some of our other areas include palliative medicine. So we have palliative medical practice, which actually focuses on pain and symptom management. Sometimes people are receiving care or treatment for something that may be a cancer treatment, but they are not really ready or not really sure if they’re ready for hospice care and we can go alongside them and work with them and help them to understand what the benefits are of palliative support, pain management support, as well as hospice support. And then we have primary care physician service. We call it our home visit physicians. And home visit physicians, allows us to visit our patients in their homes, those who are homebound and chronically ill. They’re not all necessarily hospice patients, but they just may be frail elderly who need additional support and can’t get to their doctor’s offices and other support that we can provide. We have a lot of a network of providers that we can reach out to, to help those individuals in their home from podiatry care to eye care to even their blood work can be all done through a mobile service.
Collins:
You mentioned growing up. You’ve always had a love and care for the elderly, seniors. There are many people who feel the same. What type of career paths does a Samaritan offer?
Heath:
I think that when you look at the work that we do, it’s because it’s interdisciplinary. It’s actually broader than most people think. Most people think, well, it’s just maybe you have to be a physician or you have to be a nurse to work here. But we have social workers. We have people who have chosen careers in faith based careers as chaplains or pastors, and they work here as spiritual care coordinators. We have people who have a love for seniors, but they’re not really direct care individuals, and they work in finance, they work in volunteers, departments. They work in marketing. So it’s a number of different opportunities. Where we have the greatest need is always in direct care with home health aides, with nurses, with chaplains, social workers, those positions as well.

Collins:
Okay. What’s next for Phillip W. Heath?
Heath:
Well, I think that what’s important is how we can (not just me as an individual), but we as an organization can make an impact in our community. I am a firm believer in inclusion, diversity, equity and access. And what I want to make sure is that in addition to the individuals who may traditionally have used our services, that we ensure that people in our community have access to our services. And that’s a combination of things. We hear the phrase social determinants of health these days, but people of color will tell you we’ve always had social determinants of health. We’ve been struggling with food insecurities, we’ve been struggling with transportation, we’ve been struggling with access to health care and better quality health care. And I want to ensure that we’re able to do that with the services that we offer here at Samaritan and also to partner with our community to make sure that we can achieve those things. So that’s what’s important to me is to be able to see that if someone were to ask me, you know what, what is my hope in the next 3 to 5 years? That more people have heard about the work that we do, but not just have heard about it, but have had access to care if they needed it, and if there’s opportunities for us to create opportunities for young people to develop their skill set through orientations, through trainings, through fellowships, through scholarships, we want to be able to create that.
We’re very focused on our people because without our people, we can’t do anything and we have to work together. We’re very focused on our affiliations and partnerships. We want to partner with people who may not be traditional people in our community. It may not be your traditional health care institution. It may be a human service organization or an organization just focused on children’s growth and development. And then lastly, we really want to take a look at the technology that our communities offer us, or that are available at our hands today and really take those three things to the next level. Because I think that with those things we can do amazing things in our community, particularly in health care. I had a conversation earlier today and someone was asking me about telehealth and remote patient monitoring and what does that look like? And I said, well, the way we look at it is, is there an opportunity for us to you to do it ourselves or do it with someone you know? Can we partner with someone in the community to just have better access to our services? How do we reduce food insecurity with our own patients and families? And so looking at all of those things and how they impact others.
Collins:
And these are what you consider the three big things that you look for.
Heath:
And they make up, I would say our pillars or our overarching goals that we’re trying to reach every day. And they will continue as long as long as I’m around.
Collins:
And with that said, what words of encouragement would you give to a young person that wants to pursue a career in hospice or in senior care.
Heath:
I think that the there’s probably one word that I’ve used a lot lately, and that’s just being resilient. And what I mean by that is never, never, never give up. And that’s what Winston Churchill once said. But you should never, never, never give up. Health care is challenging, but pursuit of anything is challenging. There’s a phrase that if you want something that you’ve never had, you’ve got to do something you’ve never done. And I think that’s really important as you pursue a career, whether it’s in health care or other places. But for our young people today, I say this to my son and others, you’ve got to have resilience because things don’t always work out as planned, but they always work out. And that’s an important thing.
Collins:
Okay. Let me just ask, how can people that need the services get in touch with Samaritan?
Heath:
There’s a couple of ways that people can access our services, 1-800-229-8183. Also SamaritanNJ.org, and you can learn more about us and access our services.
Collins:
In conclusion The Anointed News Journal has over 180,000 readers weekly. What do you want to say to the readers of the Anointed News Journal?
Heath:
Thank you. I will say that it’s important to keep an open mind about health care and care in general. And if you’re curious or you have a loved one that is facing a chronic illness or a serious illness, give us a call. I think that there’s a lot that we can help with. And our vision, as some of you may have seen, is helping to our patients and families to live their best life every day. And we really want to be able to do that and do that in our community.
We thank Phillip W. Heath for his perspective, and we are thankful for the impact he and Samaritan Healthcare & Hospice are making in the community. We look forward to seeing them expand their line of services.
By Chris Collins

Recent Comments